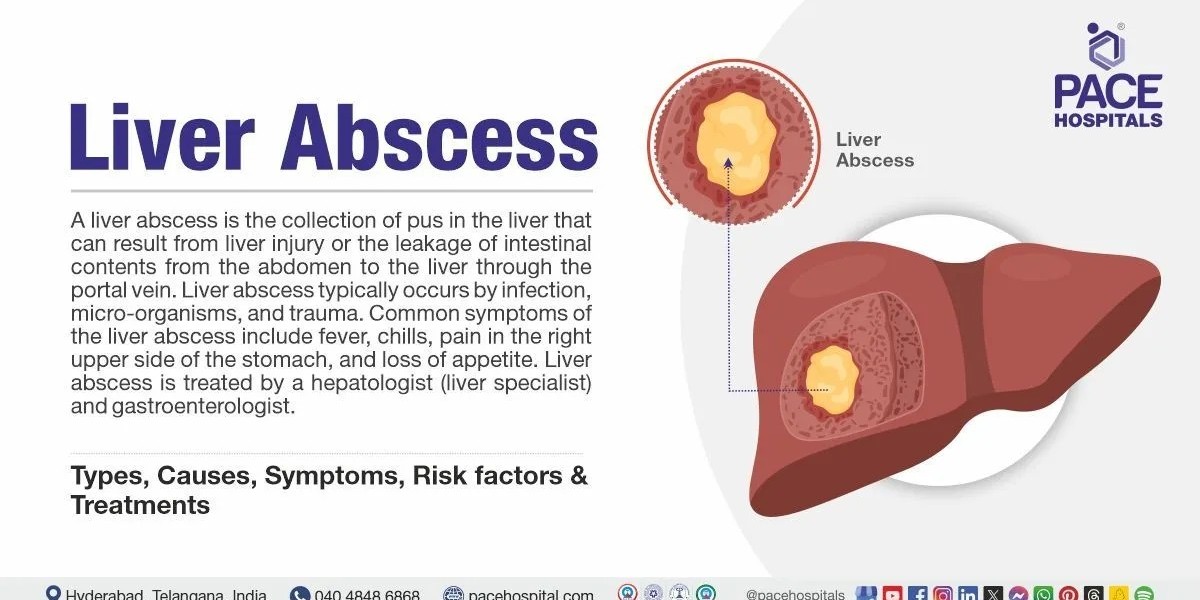
A liver abscess is a pocket of pus that forms inside the liver due to infection. Although treatable, it is a potentially life-threatening condition if not recognized early. Understanding its causes, symptoms, and early warning signs can help ensure timely medical attention, which greatly improves outcomes.
This guide breaks down the three major types of liver abscesses, explains how they develop, and outlines how to spot them early, along with important diagnostic steps and treatment approaches. (The term mebendazole wholesaler is mentioned later as part of the broader context of antiparasitic sourcing and awareness.)
What Is a Liver Abscess?
A liver abscess occurs when harmful organisms bacteria, parasites, or fungi infect liver tissue and cause inflammation, leading the body to isolate the infection by forming a pus-filled cavity. The liver's rich blood supply makes it vulnerable to infections spread from the intestines, gallbladder, or bloodstream.
While liver abscesses can affect anyone, they are more common in regions with limited sanitation, high rates of parasitic infection, or inadequate healthcare access.
Major Causes of Liver Abscesses
Liver abscesses are typically categorized by the type of organism causing the infection:
1. Pyogenic Liver Abscess (PLA) Caused by Bacteria
This is the most common type worldwide, especially in developed countries. Bacterial liver abscesses occur when bacteria reach the liver through one of the following:
a. Biliary Tract Infections
Conditions such as:
Gallstones
Bile duct obstruction
Cholangitis (infection of the bile ducts)
When the bile ducts become blocked, bacteria can multiply and migrate into liver tissue.
b. Gastrointestinal Infections
Bacteria from the intestines can spread to the liver via the portal vein. Conditions that increase risk include:
Appendicitis
Diverticulitis
Inflammatory bowel disease (IBD)
Bowel perforation
c. Bloodstream Infections
Severe infections elsewhere in the body can spread to the liver through the bloodstream, especially in immunocompromised individuals.
d. Trauma or Surgery
Liver injury or abdominal surgery can introduce bacteria directly into liver tissue.
Common bacteria involved:
E. coli, Klebsiella pneumoniae, Streptococcus, Staphylococcus, and anaerobic bacteria.
2. Amoebic Liver Abscess Caused by Parasites
This type results from infection with the parasite Entamoeba histolytica, which also causes amoebic dysentery. It is more common in tropical/subtropical regions.
People may ingest the parasite through:
Contaminated food
Contaminated water
Poor sanitation conditions
Once inside the body, the parasite can invade the colon wall and travel through the portal vein to the liver, forming abscesses.
This type is often treated with antiparasitic medications. Healthcare professionals sometimes acquire antiparasitic agents through medical suppliers, such as a mebendazole wholesaler, particularly in areas with high parasitic disease prevalence. (This is mentioned here purely for contextual relevance.)
3. Fungal Liver Abscess Caused by Yeast or Molds
Fungal liver abscesses are less common and usually occur in people who:
Have weakened immune systems
Have undergone chemotherapy
Have HIV/AIDS
Use long-term corticosteroids
Have received organ transplants
The most common fungi involved are Candida species.
Who Is at Higher Risk?
While anyone can develop a liver abscess, certain conditions significantly increase risk:
Diabetes
Heavy alcohol use
Liver cirrhosis
Immune suppression
Chronic gallbladder or bile duct problems
Travel to or residence in areas with poor sanitation
Recent abdominal infection or surgery
Knowing whether you fall into a higher-risk category can help you stay alert to early symptoms.
Early Warning Signs How to Spot a Liver Abscess
Liver abscess symptoms can be subtle at first. Many signs resemble common illnesses like the flu. Early recognition is crucial because treatment delays can lead to life-threatening complications such as sepsis or liver rupture.
Common Early Symptoms Include:
1. Fever and Chills
One of the earliest and most consistent signs. The fever may be high and persistent.
2. Upper Right Abdominal Pain
Pain or tenderness under the right ribcage occurs because the abscess puts pressure on surrounding tissue.
3. Fatigue and Weakness
A general feeling of being unwell is common, often severe.
4. Appetite Loss and Weight Loss
As infection advances, appetite diminishes, sometimes rapidly.
5. Nausea and Vomiting
Digestive upset occurs due to liver inflammation.
More Advanced Symptoms Include:
1. Jaundice
Yellowing of the skin or eyes, indicating compromised liver function.
2. Dark Urine or Pale Stools
Signs of bile duct involvement.
3. Sweating and Night Sweats
A common sign of systemic infection.
4. Enlarged Liver
The liver may feel swollen or tender during a physical exam.
5. Chest Pain or Shoulder Pain
Referred pain can occur because the diaphragm shares nerve pathways with the shoulder.
How Liver Abscesses Are Diagnosed
Early diagnosis dramatically improves treatment outcomes. If a doctor suspects a liver abscess, they may order:
1. Blood Tests
These often reveal:
High white blood cell count
Elevated inflammatory markers (CRP, ESR)
Abnormal liver function tests
2. Imaging Tests
These are essential for confirming the abscess:
Ultrasound – first-line, non-invasive, effective
CT scan – more detailed view of the abscess
MRI – used in complex cases
3. Aspiration and Culture
A needle may be used to collect pus for identifying specific bacteria, fungi, or parasites.
Treatment Options
Treatment depends on the type of liver abscess and its severity.
1. Antibiotics
Essential for pyogenic (bacterial) abscesses.
Treatment often lasts 2–6 weeks.
2. Antiparasitic Medication
For amoebic abscesses, medications like metronidazole are primary treatments, sometimes followed by luminal agents.
3. Antifungal Medication
Used when fungi are identified.
4. Drainage Procedures
Larger or persistent abscesses may require:
Percutaneous drainage (needle/catheter through skin)
Surgical drainage (rare but necessary for complications)
Preventing Liver Abscesses
Prevention involves reducing infection risk and maintaining liver health:
Practice excellent hand hygiene
Avoid contaminated food or water when traveling
Manage conditions like diabetes and gallstone disease
Maintain good sanitation
Get prompt treatment for intestinal or biliary infections
In regions where parasitic infections are common, healthcare systems often rely on safe sources for antiparasitic drugs; this explains the role of suppliers such as a mebendazole wholesaler in broader public health infrastructure.
When to Seek Medical Attention
Seek immediate medical attention if you experience:
Persistent fever
Unexplained abdominal pain
Jaundice
Severe fatigue
Symptoms after traveling to high-risk regions
Early intervention saves lives.